CALL NOW FOR A CONFIDENTIAL CONSULTATION WITH OUR PATIENT REPRESENTATIVE ATLANTA & BEVERLY HILLS 678-573-6965
Uterine Suspension – Laparoscopic Sacral Colpohysteropexy (aka Hysteropexy)
Dr Miklos & Moore most commonly perform a laparoscopic sacral colpohysteropexy (aka hysteropexy) for the treatment of uterine prolapse. To understand the procedure it is best to first understand the definition of each of the terms which make up the name of the procedure: laparoscopic sacral colpo hystero pexy (please see the box of definitions above). If one reads the simple layman definition of the terms in the list below, from bottom to top, he or she can understand what is done during the operation: ie support the uterus & vaginal vault to the tailbone using mini-incisions in the belly.
Patients have come from all over the world for Dr Miklos’ & Moores’ laparoscopic expertise and experience. The sacral colpopexy with or without a uterus in place is considered the most successful operation for the support of the vaginal vault and/or the uterus and is routinely performed via a large incision known as a laparotomy. Dr Miklos & Moore have perfected the laparoscopic approach to the sacral colpopexy and have performed more than 1200 laparoscopic sacral colpopexies since 1999. The benefits of small incisions are obvious.
Definitions of Terms
-
Laparoscopic = mini-incision in the belly
-
Sacral = tailbone
-
Colpo = vaginal vault (deepest point of vagina)
-
Hystero or Utero = uterus
-
Pexy = support
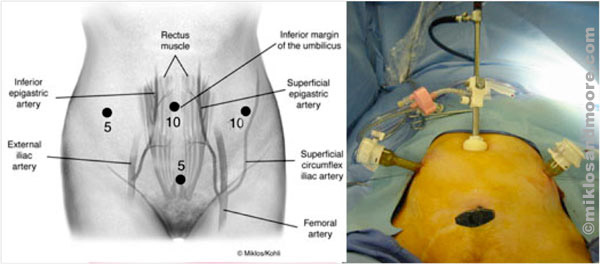
Laparoscopic Incision Sites for Hysteropexy Picture of Incision and Port Access for Hysteropexy
The causes of uterine prolapse are various and numerous. However, most consider childbirth to be the number one etiology or cause of the condition. It is not hard to imagine why when one considers the trauma childbirth can inflict on a woman’s body. The actual mechanism of action which results in uterine prolapsed is the breaking, tearing or the stretching of the uterosacral ligaments. These ligaments are what normal holds the uterus in place. They originate at the sacrum (ie tailbone) and insert or attach to the uterus. Interestingly when we do a sacral colpopexy we are using mesh to mimic the pathway of the original ligaments.
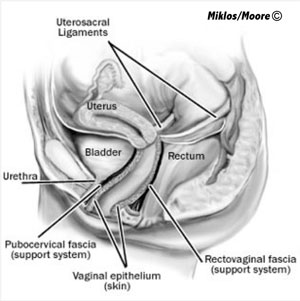
Normal Uterine Support - the uterosacral ligaments are responsible for supporting the uteruse
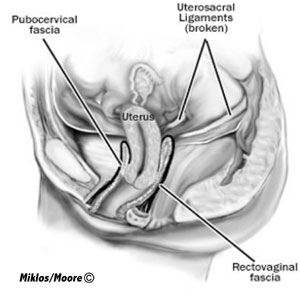
Uterine Prolapse –is a result of broken uterosacral ligaments
The laparoscopic sacral colpohysteropexy is obviously performed though the miniature incisions above using a laparoscope and TV screens. Once the laparoscopic entry ports are placed, the skin over the sacrum is dissected away.
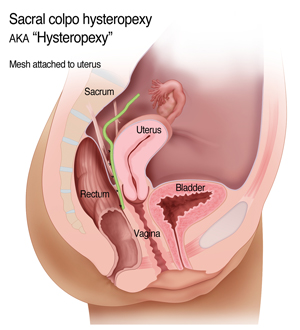
Mesh Attachment to Uterus - suturing the mesh to the posterior aspect of the uterus
Once the mesh has been secured to the back of the uterus then the mesh is secured to the sacrum using the same type of permanent suture used on the back of the uterus. The sutures don’t actually go into the bone of the sacrum, instead the attachement is to a ligament known as the presacral ligament on the bone. After the mesh is secured to the sacrum, the mesh is covered with the peritoneal skin using an absorbable suture. This helps to prevent intestines ie bowel form looping around the mesh and cause a postoperative bowel obstruction.
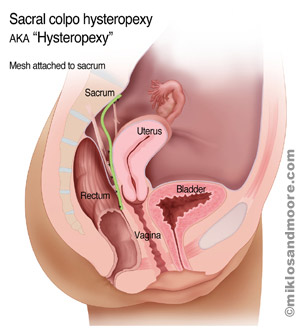
Mesh Attachment to Sacrum – sutures are placed through
the anterior ligament of the sacrum and then through the mesh; the
mesh attachment to the sacrum reestablishes uterine support
The results of repair are obvious. The mesh is now substituting for the original uterosacral ligaments, they course the same pathway from the back of the uterus up to the tailbone. Undoubtedly the mesh is even stronger than the original ligament and it is highly unusual, if the surgery has been done correctly, that the uterus could prolapse again in the future. Sacral colpopexy procedures in patients without a uterus in place (post hysterectomy) have cure rates of 96-100%. Patients with a uterus are thought to have lower cure rates of approximately 90-95% for uterine suspension. The reason is simple: if the uterus is not present or is removed, most experienced urogynecologic surgeons will use a Y-shaped mesh to attach to the apex of the vagina. Two areas of attachement provide for better support and in theory a longer lasting repair. In patients opting to keep their uterus cure rates are thought to be lower because the surgeon can really only attach mesh to one side of the uterus and more specifically the posterior vagina. This one sided attachment neglects the anterior or frontside of the apex of the vaginal vault. This anterior vaginal vault is neglected and is the area most vulnerable to prolapse in the future.
Dr. Miklos and Dr. Moore will perform laparoscopic uterine suspension surgery in most patients as long as the patient is an informed consumer and the preservation of the uterus is not detrimental to the health of the patient. Detrimental reasons include but may not be limited to: evidence of cancerous or precancerous conditions of the uterus, cervix, tubes or ovaries; symptomatic uterine fibroids; excessive menses; excessive pain during menses; central chronic pelvic pain (chronic pain from the uterus). The surgeons also want to make sure the patient understands that cure rates are thought to be higher if the no longer has a uterus and lower if the uterus remains in place.
Drs. Miklos and Moore rarely ever perform a uterine suspension surgery without correcting other vaginal prolapse defects present. It is their experience that anyone having a uterine suspension will most likely need other supportive concurrent procedures such as: a paravaginal repair (to support the ceiling of the vagina and bladder), a posterior repair (to support the floor of the vagina and rectum) and or a urethral suspension procedure (to support the ceiling of the vagina and the urethra for urinary incontinence). Dr Miklos & Moore believe in fixing all prolapsed areas concurrently in hopes of minimizing further prolapse in future. They don’t want to see a patient come back in 6 months to repair another area of the vagina which could have been fixed on her first trip to the operating room.